Welcome to the HealthSmart Pharmacy Immunisation Booking System
Phone: 03 9045 9777
* Fields marked with an asterisk must be completed
About Your Vaccination
Your appointment will take approximately 2 minutes. You can access the HealthSmart Pharmacy Privacy statement here
If you cannot attend your appointment, please reschedule it, or contact the pharmacy for a refund.
Payment is to hold your vaccine and booking - there are no refunds on cancellations except in select circumstances.
Recheduling holds your booking details and your payment.
Please note, there is a mandatory requirement for anyone who has received a vaccine to stay in the proximity of the vaccination service for 15 minutes after receiving the vaccination, so our Pharmacist Immuniser can effectively manage any adverse events following immunisation (AEFI).
During your appointment, the following will occur:
- The Pharmacist Immuniser will ask questions to ensure you are safe to have the vaccine
- In line with Australian Best Practice Standards, the Pharmacist Immuniser may not swab the skin or wear gloves before you receive your vaccination
Our Pharmacist Immuniser will administer the vaccine and provide you with a band aid or appropriate dressing.
Post vaccination wait time: 15 mins
Personal Details
General Consents
Terms & Conditions
These terms apply to the administration to you of the Vaccination from an Pharmacist Immuniser for HealthSmart. By consenting to receive the Vaccination, you confirm that you have read and agreed to the following terms:
I confirm and agree the following:
- I am the minimum required age for administering this vaccine.
- I understand that the vaccine is subject to availability.
- I have read the Consumer Medicine Information (CMI) sheet for this vaccination
- I have read and understand information on precautions, contraindications and side effects (listed in each CMI and below), am aware of and accept any risks associated with the Vaccination and to my knowledge I do not suffer from any condition or circumstance that prevents me from having the Vaccination or makes it unsafe for me.
- I will answer truthfully if the Pharmacist Immuniser asks for specific information about my health, past vaccinations or other conditions that may affect my participation.
- I will immediately inform the Pharmacist Immuniser of any adverse changes I experience in the course of participating in the Vaccination or afterwards, including (but not limited to): discomfort, pain, dizziness, shortness of breath, wheezing, difficulty breathing, swelling of the face, lips, tongue or other parts of the body.
- I understand that as part of receiving the Vaccination, HealthSmart Pharmacy must securely submit a record of my Vaccination to the Australian Immunisation Register (AIR).
- HealthSmart Pharmacy and its employees, agents, sub-contractors, directors and related bodies corporate will not be responsible for any injury, loss or damage you suffer from the Vaccination (except where liability cannot be excluded by law).
Precautions and Contraindications
I agree to let the Pharmacist Immuniser know prior to the Vaccination if I:
- have had an allergic reaction to any previous vaccine
- have recently had any other vaccine (e.g. COVID-19 vaccine)
- are allergic to the active ingredients or any other ingredients in the vaccines
- are suffering from an acute illness (e.g. an infection) or have a temperature higher than 38.5ºC
- have or have had an immune response or low immunity problem e.g. a disorder, corticosteroid, cyclosporin or cancer treatment (including radiation therapy)
- have or had allergies or allergic reactions e.g. itchy rash/hives, swelling of face, lips, mouth or tongue
- have a bleeding problem or bruise easily
- have ever fainted before, during or after having an injection
- have a known allergy to egg protein
- have a known allergy to latex, foods, preservatives or dyes
- intend to become pregnant, are pregnant or breast-feeding
- have or have had Guillain - Barre Syndrome (an illness which affects the nervous system and can cause severe muscle weakness or paralysis) after getting a flu vaccine.
I understand that having one of these issues may not prevent me from having the vaccine, but having a discussion with the Pharmacist Immuniser beforehand will allow me to make an informed choice about vaccination.
Side effects
I understand that, like all medicines, these vaccines may have some mild side effects, such as pain, tenderness, redness, swelling, bruising and hardness at the injection site, flu-like symptoms such as headaches, muscles aches, sore throat, cough, fever and chills/shivering or other symptoms like nausea, vomiting or diarrhoea.
I understand that these symptoms do not mean I am sick, they are most likely to be my body’s natural response to the vaccine. The vaccine cannot give me an illness as it does not contain any live virus. The vaccine is generally well tolerated however I should stay close by so that the nurse can keep an eye on me for 15 minutes after the vaccine.
Australian Immunisation Register (AIR) Reporting
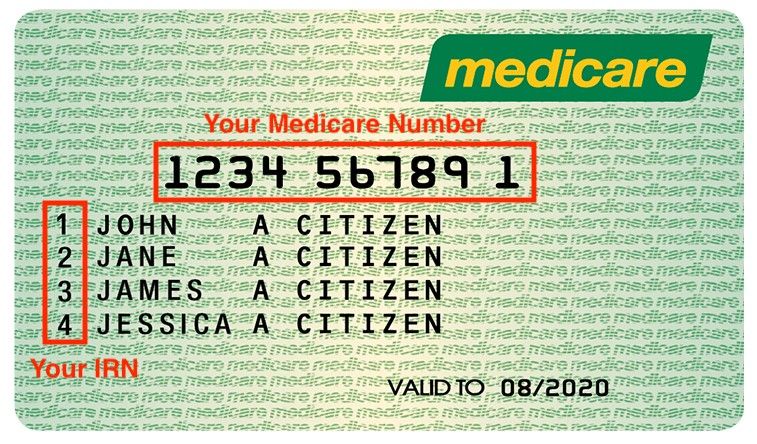
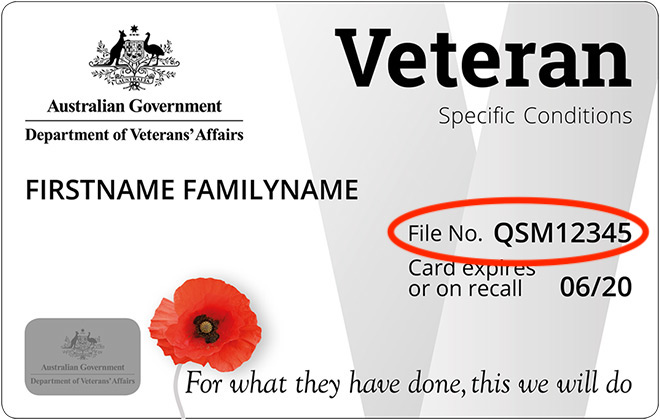
The Australian Government has introduced laws to ensure that every Australian can access their vaccine history through a safe and secure register. Vaccination providers must now report information in relation to vaccinations administered both within and outside Australia. To facilitate this reporting we may need to collect some additional personal information from you such as your Medicare details (if applicable) in order to submit a record of your Vaccination to the AIR.
Please answer all the questions ( scroll up you might have missed some questions ).